This week, we submitted comments to the U.S. Department of Health and Human Services (HHS) in response to the agency’s proposed rule to expand the availability of short-term, limited duration insurance (STLDI) plans. This rule would mean millions of people would have bad insurance plans that do not cover their health needs and millions more would be paying much higher prices for quality coverage.
Read More
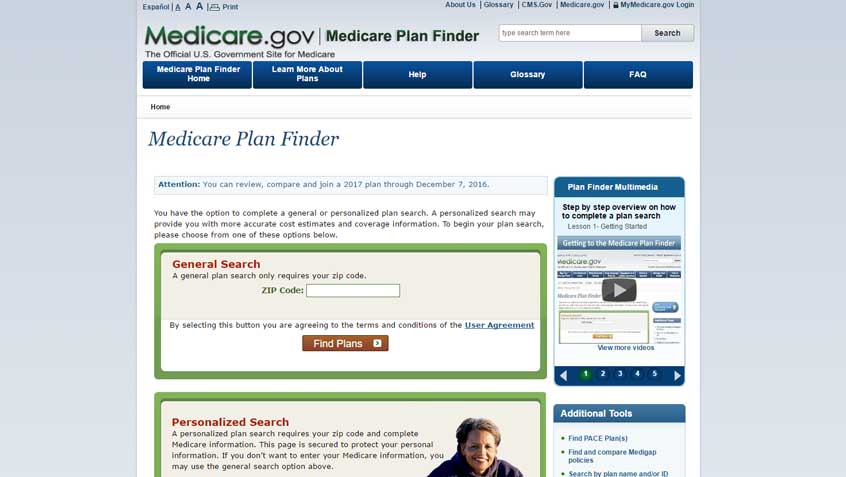
This week, the National Council on Aging (NCOA) and the Council for Affordable Health Coverage’s Clear Choices Campaign released a long-anticipated report on the Medicare Plan Finder (MPF) tool. The Modernizing Medicare Plan Finder Report highlights some of the issues Medicare beneficiaries, their families, and their caregivers encounter while using the MPF tool as well as future considerations for the tool’s development and recommendations for improvement.
Read More
On January 11, 2018, the Centers for Medicare & Medicaid Services (CMS) issued guidance announcing a new policy that, for the first time, will allow states to make participation in a work or “community engagement” program a condition for Medicaid enrollment. The next day, CMS approved a Medicaid waiver in Kentucky that will allow the state to test this new policy.
Read More
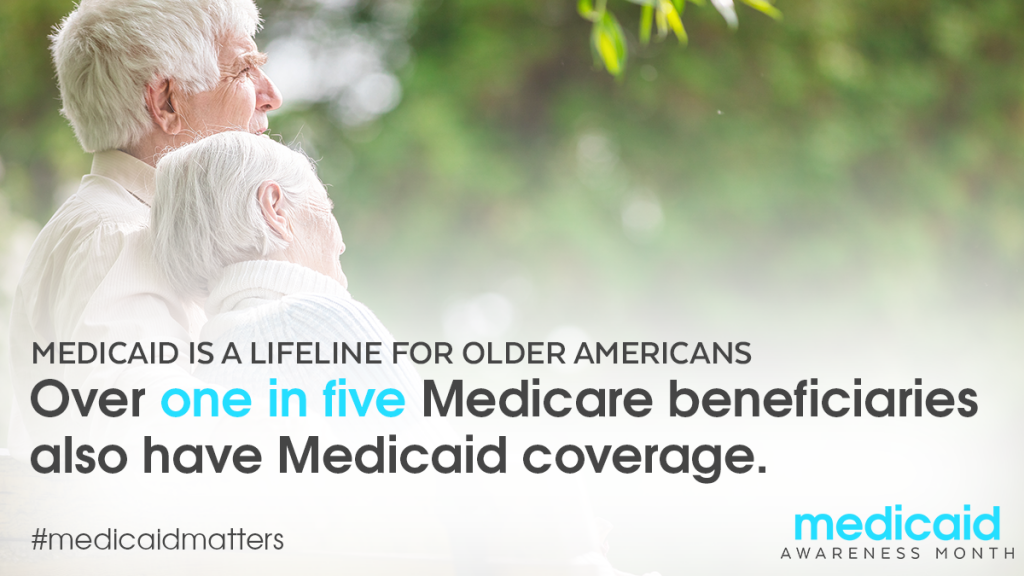
This month, stakeholders and advocates across the country are observing Medicaid Awareness Month. Organized by the Protect Our Care coalition, the month-long campaign is intended to enhance awareness of the many ways the Medicaid program strengthens American communities.
To that end, the coalition is launching outreach and education efforts on a different topic each week. These activities will culminate in a national Medicaid Day of Action on April 30.
Read More
The recently-passed Bipartisan Budget Act of 2018 (BBA of 2018) makes a number of changes to Medicare, including permanently authorizing Dual Special Needs plans (D-SNPs), which are Medicare Advantage (MA) plans for people who are dually eligible for Medicare and Medicaid.
To help inform implementation of these changes, earlier this month the Centers for Medicare & Medicaid Services (CMS) issued a request for stakeholder input on (1) The design of an integrated Medicare-Medicaid appeals approach for D-SNPs; and (2) The establishment of minimum state contract requirements for D-SNPs.
Read More
Over the past few months, the Medicare Rights Center has been actively engaged in considering and commenting on proposals from the Centers for Medicare & Medicaid Services (CMS) that could have significant effects on people who are enrolled in Medicare Advantage (MA) and Part D plans. Last week, CMS released both the Contract Year 2019 Final Rules for Medicare Advantage and Part D (Final Rules) and the 2019 Call Letter. CMS also released fact sheets for the Final Rule and the Call Letter. As we continue to analyze the Final Rules and Call Letter, as well as the impact of the recent two-year budget deal, here is a preview of the issue areas we intend to spotlight, which focus on regulatory trends, anticipated implementations, and practical changes that will impact people with Medicare and those who help them navigate coverage decisions.
Read More
The Kaiser Family Foundation recently published a list of frequently asked questions about the Center for Medicare and Medicaid Innovation (CMMI) within the Centers for Medicare & Medicaid Services (CMS).
Also known as the “Innovation Center” CMMI was created by the Affordable Care Act to test new ways to improve care and lower costs within Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP).
Read More
This week, the Centers for Medicare & Medicaid Services (CMS) released the final Medicare Advantage and Part D 2019 Rate Announcement and Call Letter. This is the finalized annual update to Medicare Advantage and Part D programs, which includes payment updates and policy changes for payment in calendar year (CY) 2019.
Read More