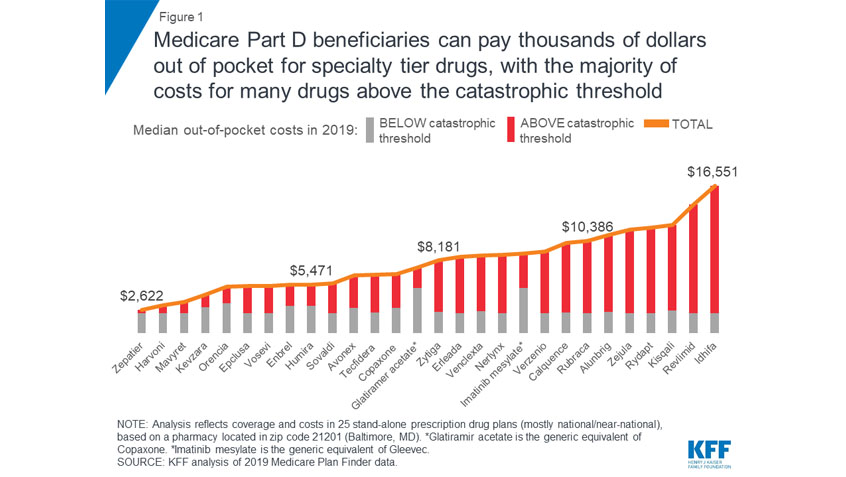
While Medicare Part D has made prescription drugs more affordable for people with Medicare, many beneficiaries continue to face affordability challenges, in part because there is no hard cap on out-of-pocket spending under Part D. A new resource from the Kaiser Family Foundation examines the financial burden this places on Part D enrollees who rely on high-cost medications.
Read More
On January 1, 2019, the durable medical equipment (DME) competitive bidding program temporarily ended.
The competitive bidding program was originally designed to reduce out-of-pocket expenses and help ensure that people with Medicare had access to quality DME, supplies, and services from suppliers they could trust. The program benefited people who had Original Medicare, lived in a competitive bidding area, and needed DME that fell under the competitive bidding program.
Read More
This week, the Centers for Medicare & Medicaid Services (CMS) )—the agency that oversees the Medicare program—announced a new model to test changes to prescription drug payments and incentives. The CMS Center for Medicare and Medicaid Innovation (CMMI) will create a voluntary, five-year model in which Part D Plans (PDPs) and Medicare Advantage Prescription Drug Plans (MAPDs) may apply to participate.
According to CMS, the model is intended to test “new incentives for plans, patients, and providers to choose drugs with lower list prices in order to address rising federal reinsurance subsidy costs.”
Read More
Last week, the Centers for Medicare & Medicaid Services (CMS)—the agency that oversees the Medicare program—announced that they finished the rollout of new Medicare cards to 61 million people with Medicare ahead of the original deadline of April, 2019. This means that all people with Medicare should now have Medicare cards that include a random Medicare Beneficiary Identifier (MBI) instead of a number based on their Social Security number.
Read More
As the government shutdown continues, so do its impacts on older adults, people with disabilities, and their families. While Medicare and Medicaid are fully funded for the year, other critical programs—like affordable housing, food assistance, and transportation services—are not. This threatens the health and economic security of millions of Americans.
Read More
Older adults and people with disabilities who are currently enrolled in a Medicare Advantage (MA) plan have until March 31 to switch to another MA plan or to Original Medicare with or without a stand-alone prescription drug plan (Part D) during the new Medicare Advantage Open Enrollment Period (MA OEP).
The MA OEP occurs each year from January 1 through March 31, and it is only available to people who have a Medicare Advantage plan. One change can be made during this period, which will take effect the first of the month following the month you enroll. For example, if you switch to a new Medicare Advantage Plan in February, your new coverage begins March 1.
Read More
In November, the Centers for Medicare & Medicaid Services proposed regulatory changes to the Affordable Care Act’s Health Insurance Marketplaces. We submitted comments this week, in which we raise concerns with several aspects of the proposed rule that could have negative implications for people with Medicare.
CMS indicates it is proposing this rule in part to ensure that people are in the “most appropriate type of coverage.” While Medicare Rights supports this goal, we disagree with the agency’s proposal to achieve it by automatically terminating Marketplace coverage for people who are eligible for or enrolled in Medicare Part A.
Read More
As 2019 gets underway, the Medicaid program continues to be in the spotlight. This week, the Kaiser Family Foundation (KFF) released an issue brief that highlights some of the major program changes that states, the Administration, and Congress may pursue in 2019.
Over 66 million people receive their health coverage through Medicaid, including older adults, people with disabilities, children, low-income parents, and other adults. Any changes to the program, therefore, have the potential to affect millions of families.
Read More
In November, the Centers for Medicare & Medicaid Services (CMS)—the agency that oversees the Medicare program—announced new proposals that could potentially lower prices for some of the drugs covered by Medicare Part B but could threaten access to medications for people with Medicare. CMS invited comment on their proposals and, last month, Medicare Rights responded.
Health care affordability is a top issue on our national helpline each year, and the high cost of prescription drug coverage is one major component of this. Most of the medications people with Medicare take are covered under Part D. Part B only accounts for a small percentage of Medicare-covered drugs, but they are some of the most expensive. It is clear that Part B medications can drive significant out-of-pocket costs for people with Medicare with life-altering conditions like cancer, end-stage renal disease, or rheumatoid arthritis.
Read More
The Medicare Rights Center recently submitted comments in response to proposed rule changes from the Center for Medicare & Medicaid Services (CMS) pertaining to Medicare Parts C and D for 2020 and 2021. Many of the proposed rules implement changes that Congress made to the law that establishes Duals Special Needs Plans (D-SNPs). D-SNPs are special plans designed to serve the needs of people who are eligible for both Medicare and Medicaid, also known as “dual eligibles.”
Read More