Early Issues Around Medicare Plan Finder Data Resolved
Missing information is always a problem, but in a year where additional assistance may not be as available as usual, these gaps in reported information from plans present particular challenges.
Take Action: Tell your senators to reject harmful cuts to health care!


Missing information is always a problem, but in a year where additional assistance may not be as available as usual, these gaps in reported information from plans present particular challenges.

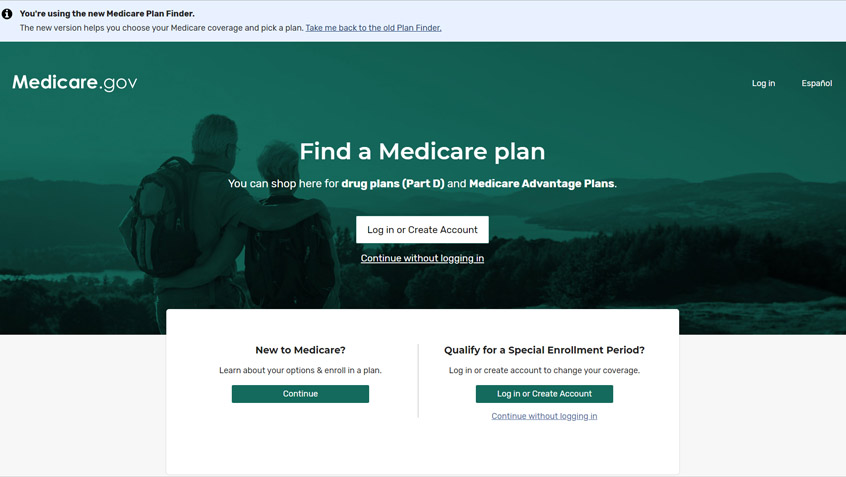
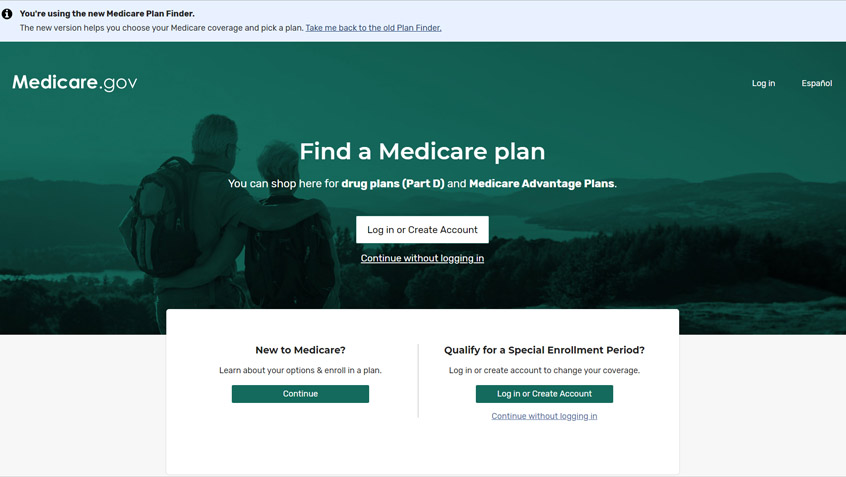
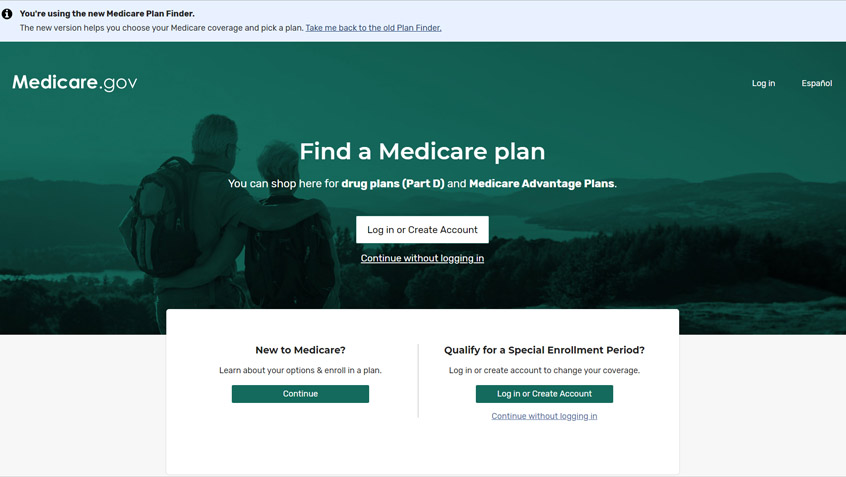
Each year, during Fall Open Enrollment (October 15 through December 7), people with Medicare have the opportunity to make certain changes to their coverage, including switching prescription drug plans or between Original Medicare and Medicare Advantage (MA).

Yesterday, Congress passed and the President signed a bill that funds the federal government through December 11, setting the stage

Census data released last week show that the number of uninsured Americans has been on the rise in recent years. The share of those who were uninsured at the time of the survey grew for the third year in a row, even as the economy was growing.

This new approach will help eligible New Yorkers get enrolled in the MSP with fewer administrative hurdles and delays and should serve as a model for other states to improve efficiency and increase enrollment in these essential programs.

This week, the Commonwealth Fund released a report that summarizes and analyzes the over 200 temporary legislative and regulatory changes that have been made to Medicare in response to the COVID-19 public health emergency. They also looked at the sub-regulatory guidance that the Centers of Medicare & Medicaid Services (CMS) has released to interpret these rules and to provide additional flexibility to providers and Medicare plans.
The Centers for Medicare & Medicaid Services (CMS) and the Social Security Administration (SSA) recently expanded the functionality of the Medicare enrollment process to accommodate more online applications during the coronavirus pandemic.

This week, the Centers for Medicare & Medicaid Services (CMS) announced new opportunities for people to enroll in Medicare or make certain changes to their coverage during the coronavirus emergency. While these temporary policies are a step in the right direction, they are too narrow and leave some without relief. More needs to be done.

The Kaiser Family Foundation recently released a report detailing how financially secure or insecure Medicare beneficiaries were in 2019. Consistent with previous years, the report shows that any stereotype of baby boomers as uniformly affluent is deeply misguided. Instead, half of people with Medicare have incomes below $29,650 and one in four live on less than $17,000. Savings rates are similarly dire. Half of Medicare beneficiaries have below $73,000 in resources, one in four has less than $8,300, and about 1 in 9 has no savings or is in debt. They also face significant out-of-pocket health care expenses in absolute terms and as a percentage of their income.
The Social Security and Medicare Trustees reports were released this week. The reports include short- and long-term projections for the financial situation of the Social Security Retirement and Disability and the Medicare HI (Part A) and SMI (Part B) trust funds. The findings are largely consistent with those from 2019 and confirm the Medicare and Social Security programs are strong and built to last.
Missing information is always a problem, but in a year where additional assistance may not be as available as usual, these gaps in reported information from plans present particular challenges.

Each year, during Fall Open Enrollment (October 15 through December 7), people with Medicare have the opportunity to make certain changes to their coverage, including switching prescription drug plans or between Original Medicare and Medicare Advantage (MA).

Yesterday, Congress passed and the President signed a bill that funds the federal government through December 11, setting the stage

Census data released last week show that the number of uninsured Americans has been on the rise in recent years. The share of those who were uninsured at the time of the survey grew for the third year in a row, even as the economy was growing.

This new approach will help eligible New Yorkers get enrolled in the MSP with fewer administrative hurdles and delays and should serve as a model for other states to improve efficiency and increase enrollment in these essential programs.

This week, the Commonwealth Fund released a report that summarizes and analyzes the over 200 temporary legislative and regulatory changes that have been made to Medicare in response to the COVID-19 public health emergency. They also looked at the sub-regulatory guidance that the Centers of Medicare & Medicaid Services (CMS) has released to interpret these rules and to provide additional flexibility to providers and Medicare plans.
The Centers for Medicare & Medicaid Services (CMS) and the Social Security Administration (SSA) recently expanded the functionality of the Medicare enrollment process to accommodate more online applications during the coronavirus pandemic.

This week, the Centers for Medicare & Medicaid Services (CMS) announced new opportunities for people to enroll in Medicare or make certain changes to their coverage during the coronavirus emergency. While these temporary policies are a step in the right direction, they are too narrow and leave some without relief. More needs to be done.

The Kaiser Family Foundation recently released a report detailing how financially secure or insecure Medicare beneficiaries were in 2019. Consistent with previous years, the report shows that any stereotype of baby boomers as uniformly affluent is deeply misguided. Instead, half of people with Medicare have incomes below $29,650 and one in four live on less than $17,000. Savings rates are similarly dire. Half of Medicare beneficiaries have below $73,000 in resources, one in four has less than $8,300, and about 1 in 9 has no savings or is in debt. They also face significant out-of-pocket health care expenses in absolute terms and as a percentage of their income.
The Social Security and Medicare Trustees reports were released this week. The reports include short- and long-term projections for the financial situation of the Social Security Retirement and Disability and the Medicare HI (Part A) and SMI (Part B) trust funds. The findings are largely consistent with those from 2019 and confirm the Medicare and Social Security programs are strong and built to last.