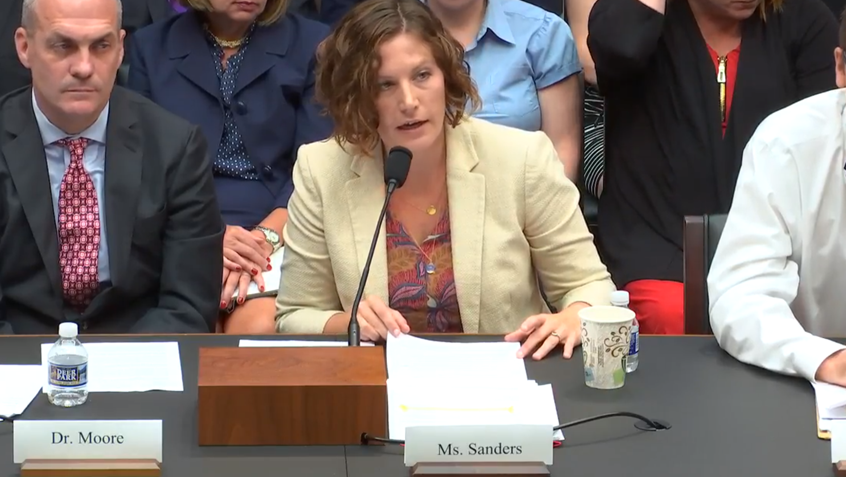
Medicare Rights Testifies at Congressional Hearing on Medicare Fraud and Abuse
Today, Stacy Sanders, federal policy director of the Medicare Rights Center, testified in support of a proposed law that would increase the civil monetary penalties and criminal fines for certain types of Medicare fraud at a hearing held by the Subcommittee on Health of the U.S. House Committee on Energy and Commerce. The hearing focused on a number of bipartisan bills to improve Medicare, including the Medicare Civil and Criminal Penalties Update Act of 2017 (H.R. 3245).









