Medicare Rights Highlights Opportunities to Improve Care for Dually Eligible New Yorkers
People who are eligible for both Medicare and Medicaid have diverse needs and circumstances. However, nearly all face challenges navigating their coverage because being enrolled in both programs means working with two sets of benefits, rules, processes, and providers.
There is federal and state interest in improving care integration for this population, such as the Centers for Medicare & Medicaid Services (CMS) Financial Alignment Initiative. This initiative tests state models like New York’s Integrated Appeals and Grievances demonstration, to better coordinate care for dually enrolled individuals.
In addition, there have been recent administrative changes, recommendations for Congress and states from the CMS Medicare-Medicaid Coordination Office, and corresponding policies in several presidential budget requests, including one that would build on the New York demo by further unifying Medicare and Medicaid appeals procedures.
Congress has focused on integration for this population in working groups, information requests, hearings, and legislative proposals. Despite all these efforts, comprehensive and fully successful reforms remain elusive. As this work continues, a new report from the Medicare Rights Center examines recent integration efforts in New York, including policy pitfalls and beneficiary-centered solutions.
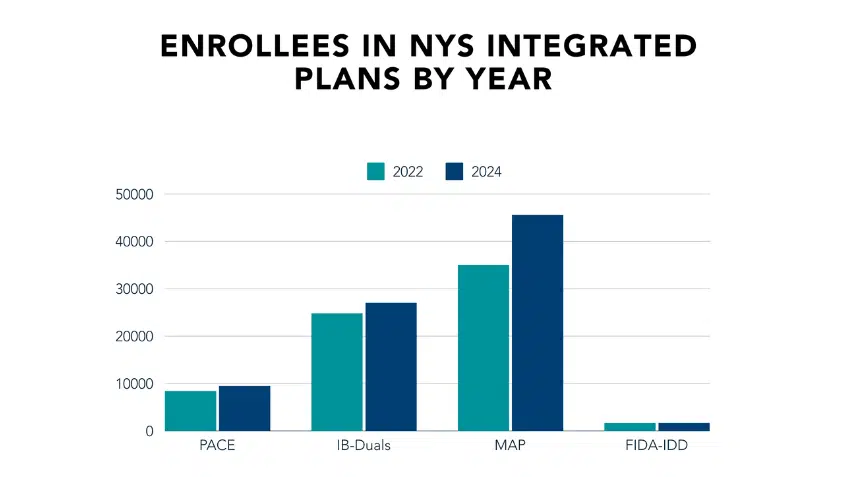
In 2022, New York released a Dual Eligible Integrated Care Roadmap, outlining Medicare-Medicaid coordination priorities intended to improve health outcomes, enhance enrollee satisfaction, and reduce costs. One of the state’s most ambitious goals was a 250% increase in the number of dually eligible individuals receiving integrated care through an aligned contract (meaning the individual’s Medicare and Medicaid benefits are provided by the same company) by the end of 2023. New York has yet to reach this target, but it may do so in the coming years—enrollments in integrated care options have increased by 30% since 2020.
Unfortunately, even while New York seeks greater enrollment into integrated care products, the state and insurers have failed to address several issues around outreach, enrollment, and coverage that could improve enrollee health and wellbeing. Every year, through the Medicare Rights Center’s national helpline, we counsel thousands of dually eligible individuals, providing information about coverage options, troubleshooting enrollment problems, assisting in provider searches, and much more. Based on this experience, we know these problems are systemic, and that further reforms are needed to truly advance coverage and care for dually eligible New Yorkers.
The report explores these challenges and presents the following recommendations to New York policymakers:
- Develop culturally competent educational and counseling resources that explain integrated care options in consumer-friendly ways.
- Prevent harmful unintended consequences of enrollment changes, such as coverage losses and higher costs.
- Set a goal of 100% network congruency for a type of Medicare Advantage plan called a Dual Eligible Special Needs Plan (D-SNP).
- Ensure D-SNPs provide clear explanations of benefits, including identifying which benefits come from the individual’s Medicaid enrollment and which are attributable to the plan.
- Require aligned D-SNPs to meaningfully coordinate Medicare and Medicaid services, including by having a “no wrong door” policy when members contact either the D-SNP or the Medicaid plan.
- Strengthen stakeholder engagement. For example, by creating a stakeholder advisory committee and dedicated office within the Department of Health that is focused on dually eligible individuals.
Medicare Rights supports the aims of integration and applauds New York for creating the 2022 Roadmap and prioritizing the needs of Medicare-Medicaid enrollees. It is unclear whether the state plans to update the Roadmap for 2024 and beyond, as there have been many changes to the integrated care landscape since its original publication. Nevertheless, Medicare Rights hopes these recommendations can aid policymakers nationwide as they determine future integrated care priorities.
Read the report, Improving Integrated Care for the Dually Eligible: Recommendations for New York.
For more information on D-SNPs, see a Medicare Rights fact sheet and video on the Promise and Pitfalls of Dual Eligible Special Needs Plans (D-SNPs). To learn more about Medicare Advantage plans and why reforms are needed, view the full Medicare Advantage 101 policy series.
The Latest
Most Read
Congress Moves to Cut Medicaid
Threats to the Social Security Administration and to Benefits Continue to Raise Alarm
House Adopts Senate Budget Plan, Laying the Groundwork for Significant Health Care Cuts
Trump Administration and DOGE Eliminate Staff Who Help Older Adults and People With Disabilities
Add Medicare to Your Inbox
Sign up to receive Medicare news, policy developments, and other useful updates from the Medicare Rights.
View this profile on InstagramMedicare Rights Center (@medicarerights) • Instagram photos and videos









