Medicare Advantage Pulling in Billions in Dubious Quality Bonuses

The Medicare Rights Center’s policy series, Medicare Advantage 101, covers the history of and issues within Medicare Advantage (MA), including overpayments to the program that burden Medicare, beneficiaries, and taxpayers.
One driver of these overpayments is a controversial system called the Quality Bonus Program (QBP). As we have outlined before, the QBP requires the Centers for Medicare & Medicaid Services (CMS) to rate plans in every county on a five-star system. Plans that score at least 4 stars get a bonus payment. In some counties, plans can get their bonuses doubled.
The QBP was created to reward high-quality plans and help people make informed decisions. But plan scores keep creeping up across the board, leaving shoppers with little to compare and fewer clues about which plans are the best fit for them. And, due to issues with the underlying metrics, it is unclear if the plans with higher scores genuinely have better quality. For example, Medicare Rights and others have observed that the QBP star ratings contain too many measures, diluting their relevance, and are not a useful tool for enrollees anyway because they are contract, rather than plan, specific. As the Medicare Payment Advisory Commission (MedPAC) said in 2023: “The current state of quality reporting is such that the Commission’s yearly updates can no longer provide an accurate description of the quality of care across MA plans.” Yet plan ratings, and bonus payments, continue to rise.
A new report from KFF shows these trends remain entrenched. As illustrated in the KFF graphic below, payments have varied a bit in the past few years due to erratic effects from the COVID-19 public health emergency but have shown a general upward trend. In 2022, they were around $10 billion, leaping to $12.8 billion in 2023. In 2024, the QBP is expected to pay out at least $11.8 billion. However, it is unclear if the surge in highly rated, highly paid plans is due to meaningful quality improvements or a ratings system that is inaccurate, ineffective, and easily manipulated.
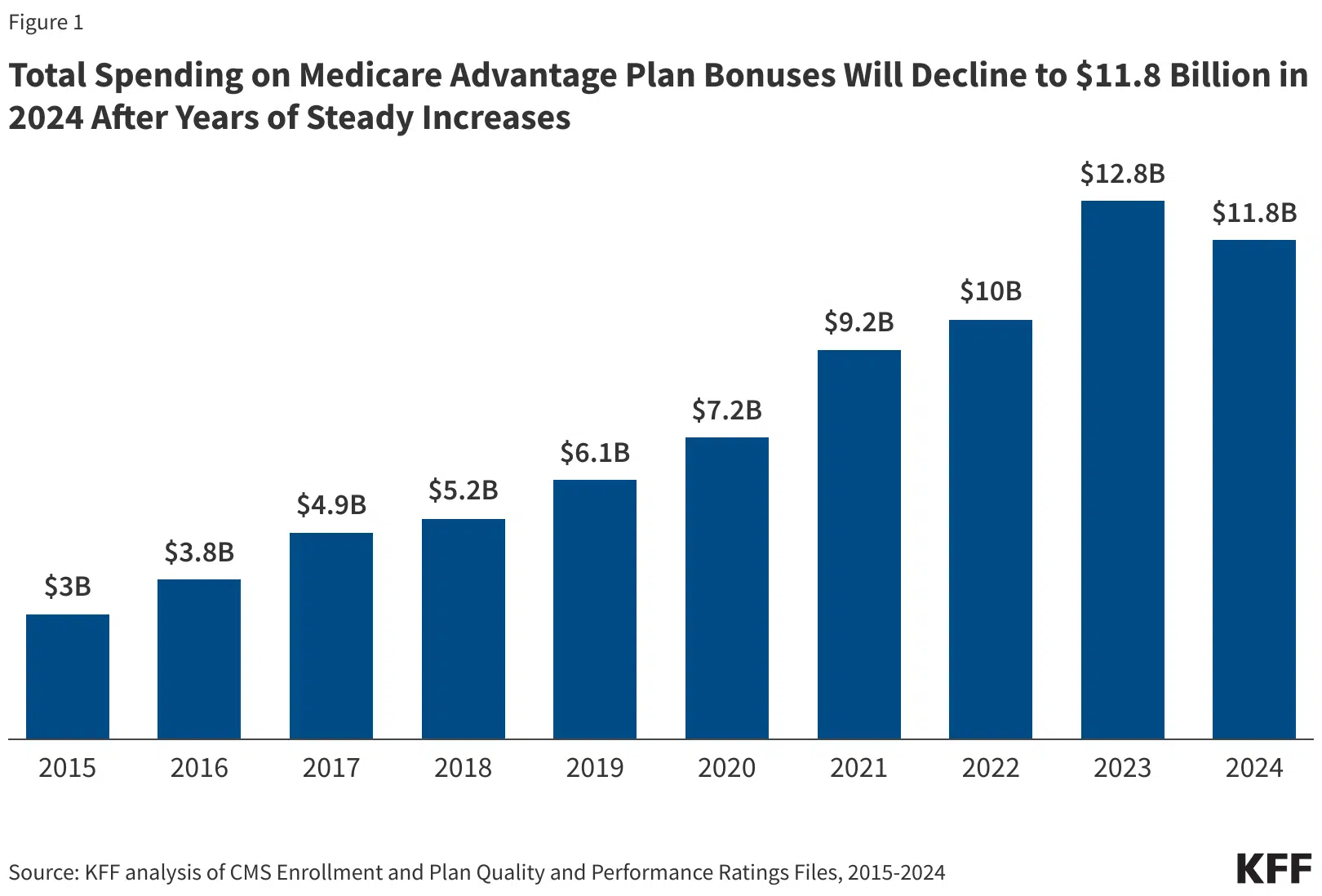
Although the QBP’s relationship to plan quality is questionable, its effect on Medicare costs is not. Since 2015, the program has paid out around $74 billion in bonuses. And unlike other quality programs, the QBP is not required to be budget neutral. That allows payments to simply keep growing and gives plans carte blanche to game a broken system and collect ever-larger sums of unwarranted Medicare dollars.
Absent significant reforms, these problems will only escalate. At Medicare Rights, we think it is past time to revise or replace the QBP, curtail MA overspending more generally, and increase oversight and enforcement for MA plans.
Read more about how MA payment rates are set, including QBP payments.
Read about other MA topics in our MA 101 series.
The Latest
Most Read
Congress Moves to Cut Medicaid
Threats to the Social Security Administration and to Benefits Continue to Raise Alarm
House Adopts Senate Budget Plan, Laying the Groundwork for Significant Health Care Cuts
Trump Administration and DOGE Eliminate Staff Who Help Older Adults and People With Disabilities
Add Medicare to Your Inbox
Sign up to receive Medicare news, policy developments, and other useful updates from the Medicare Rights.
View this profile on InstagramMedicare Rights Center (@medicarerights) • Instagram photos and videos









