House Republicans Move Forward with Plans to Cut Medicaid and Food Stamps, Reducing Coverage for Millions
On Tuesday, three House committees moved forward with agendas that would make it harder for older adults, people with disabilities,
Join Us Live for a Discussion on Medicare, Democracy, and the Future of Health Care
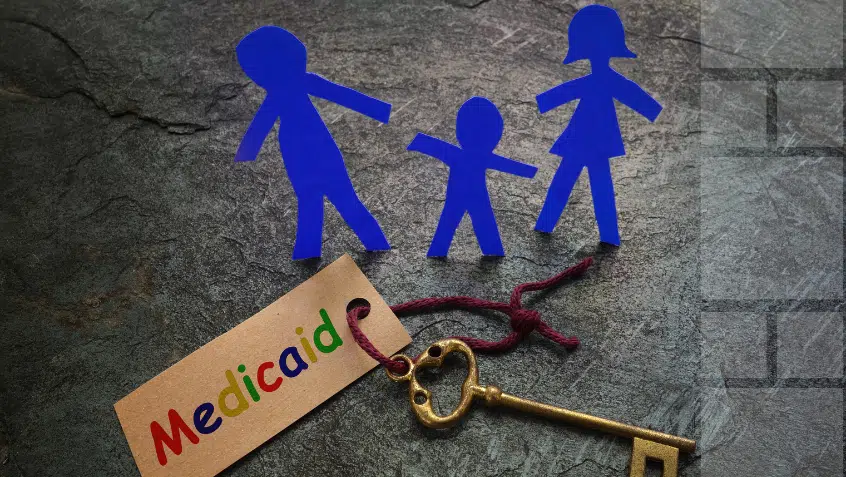
Distinct Medicare and Medicaid rules, funding streams, and service delivery systems can create barriers that increase costs and worsen outcomes for people who are jointly enrolled in the programs. We support correcting this fragmentation through policies that offer meaningful choice; reduce disparities in access to and quality of care; rely on active and informed enrollee participation; include robust safeguards and oversight; offer clear enrollee and provider education about options for accessing integrated care; establish unified grievance and appeals processes; ensure seamless access to data; and provide person-centered care coordination and care management.
On Tuesday, three House committees moved forward with agendas that would make it harder for older adults, people with disabilities,

–Statement by Medicare Rights Center President Fred Riccardi– New York, NY—House Republicans have now unveiled their proposals to slash Medicaid

This week, the non-partisan Congressional Budget Office (CBO), a Congressional agency that conducts independent analyses of economic and budget issues,

Back from a two-week recess, House Republicans took concrete steps this week towards crafting a reconciliation bill. The chamber hopes

Through a series of widely reported moves, the Trump administration, through Elon Musk’s Department of Government Efficiency (DOGE), is hamstringing

The House of Representatives advanced a harmful budget blueprint last week that analysts and advocates said would result in devastating
Without Medicaid, many Medicare enrollees—especially those with limited income—would struggle to afford care, risking their health or having to choose between medical care and housing, food and other essentials. Cutting Medicaid would directly harm millions of Medicare enrollees and increase costs for the Medicare program and state budgets.

Late Tuesday, House Republicans narrowly passed their budget resolution, paving the way for a reconciliation bill that advances key Trump

In a disappointing vote Tuesday, Republicans in Congress have decided to move forward with plans to cut Medicaid. As we
Medicaid is health insurance, long-term care coverage, and a workforce program all in one. It is a lifeline that helps
On Tuesday, three House committees moved forward with agendas that would make it harder for older adults, people with disabilities,

–Statement by Medicare Rights Center President Fred Riccardi– New York, NY—House Republicans have now unveiled their proposals to slash Medicaid

This week, the non-partisan Congressional Budget Office (CBO), a Congressional agency that conducts independent analyses of economic and budget issues,

Back from a two-week recess, House Republicans took concrete steps this week towards crafting a reconciliation bill. The chamber hopes

Through a series of widely reported moves, the Trump administration, through Elon Musk’s Department of Government Efficiency (DOGE), is hamstringing

The House of Representatives advanced a harmful budget blueprint last week that analysts and advocates said would result in devastating
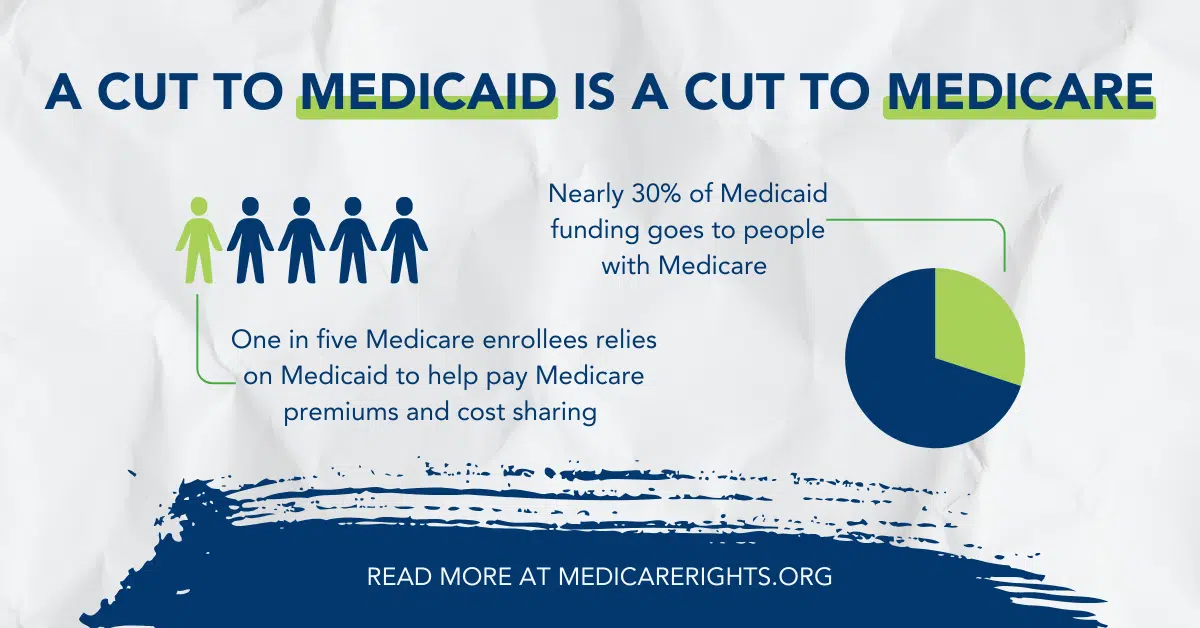
Without Medicaid, many Medicare enrollees—especially those with limited income—would struggle to afford care, risking their health or having to choose between medical care and housing, food and other essentials. Cutting Medicaid would directly harm millions of Medicare enrollees and increase costs for the Medicare program and state budgets.

Late Tuesday, House Republicans narrowly passed their budget resolution, paving the way for a reconciliation bill that advances key Trump

In a disappointing vote Tuesday, Republicans in Congress have decided to move forward with plans to cut Medicaid. As we
Medicaid is health insurance, long-term care coverage, and a workforce program all in one. It is a lifeline that helps